The Pituitary Neuro-Ophthalmic Approach
How well do you know it?...
In ophthalmic medicine, our proper understanding of the "how & why" of neuro-ophthalmic concepts is key in diagnosis, prognosis, and management of pituitary conditions, particularly in scenarios involving potential compressive mass effects.
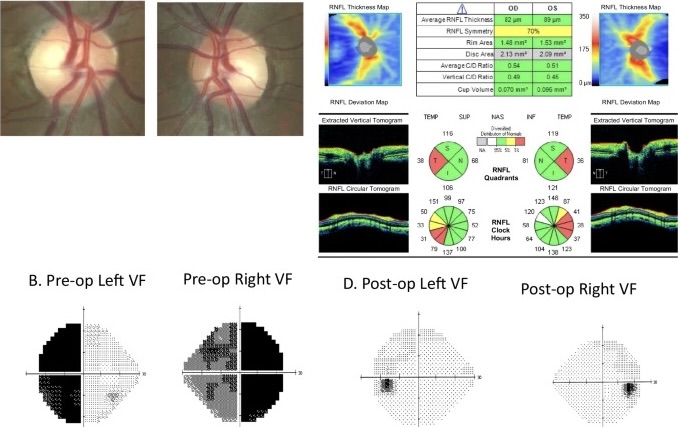
Optical coherence tomography (OCT) has also revolutionized our approach, offering us never-before insight into structural changes associated with chiasmal compression. OCT parameters, such as peripapillary retinal nerve fiber layer (pRNFL) and macular ganglion cell complex (mGCC) measurements, not only help us in early detection but also provide powerful prognostic clues for visual recovery post-surgery.
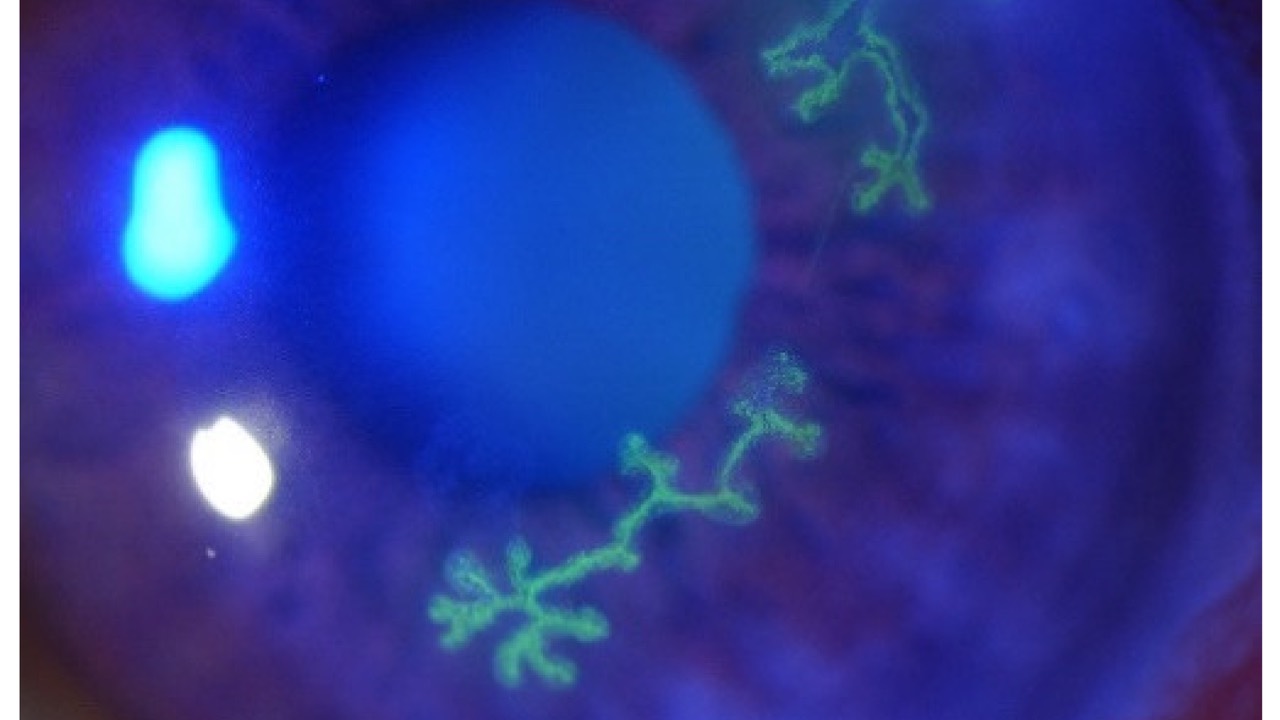
Well known neuro-ophthalmic consequences of pituitary mass effect & compression include visual field deficits (the infamous bitemporal hemianopia), "upstream" optic neuropathy, impaired color perception, as well as potential optic atrophy with decreased visual acuity. However, purely EOM cranial nerve palsies and diplopia can also occur depending on its anatomical presentation and course. So it's important to know the presentation can vary significantly, with many individuals being absolutely asymptomatic early on due to its usual insidious nature.
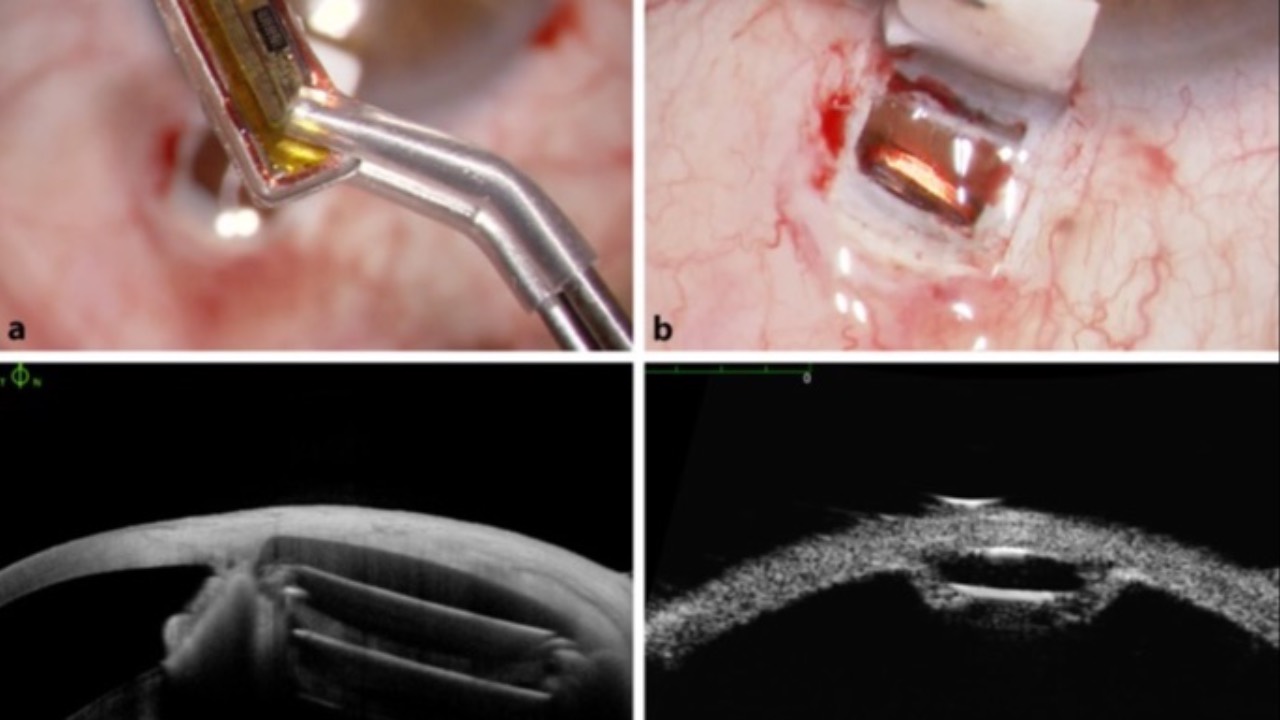
Management strategies for space-occupying compressive pituitary lesions (most common is prolactinoma) must be multidisciplinary. While surgical resection is the primary intervention for significant chiasmal mass effect, the timing and approach of surgery is often guided by neuro-ophthalmic findings. And pre-operative OCT measurements, particularly pRNFL thickness, have been shown to be strong predictors of post-operative visual outcomes. For example, individuals with pre-operative pRNFL measurements above the fifth percentile of age-matched norms experience more rapid visual field recovery post-surgery.
Interdisciplinary communication between those of us in ophthalmic medicine, endocrinologists, and neurosurgeons is key in managing pituitary compression effectively. Our long-term neuro-ophthalmic management is of course very important in terms of OCT and/or visual field changes, which may be the first sign of recurrence or secondary complications such as chiasmal descent or adhesions. Our regular post-ops, ideally at 3-12 month intervals, should include comparative OCT's, visual fields, color, and of course VA's.
By leveraging these in-office diagnostics each of us should have easy access to, keeping a collaborative approach, we play a very important role in the likelihood of positive outcomes for our patients over time.
-JRM
Go to the article in Nature Eye HERE.
VISION & NEUROLOGY CASEBOOK BUNDLE
NEW! Downloadable Book & Podcast Bundle
Whether you’re an optometrist, ophthalmologist, family physician, or simply fascinated by the science of vision and the brain, this casebook and podcast provides practical insights and real-world scenarios which will enhance your clinical knowledge.
Check out the Downloadable Book & Podcast Bundle (with bonuses)!...
PUBLISH YOUR EXPERIENCE
BUILD A CE/CME ONLINE COURSE FROM MATERIAL YOU ALREADY HAVE!
- No Fees: We'll build & publish your course on our powerful platform.
- Income Stream: We do the work & you earn.
- Real Partnership: Real humans.
- Utilize Existing Materials: Notes, FAAO papers, writings collecting dust?
- Share Your Expertise: Teach others to help others.
- Global Audience: Reach eager learners worldwide.
- Advance Your Career: Contribute to ophthalmic medical education.





Responses